Hidden contributor of pain in clinical practice – “Catastrophizing”
The experience of pain is a complex interplay between psychological, biological, and cultural factors [1]. Individual who experience pain from any surgical procedure or from any injury to the tissue tends to distress or pain. But question arises why the person with same type of injury or surgery tend to have different level of pain intensity? It depends on the extent of the injury, the type of tissue damage and the cognitive factors including - catastrophizing. Individuals who have high level of pain have a tendency to magnify or exaggerate the threat value or seriousness of the pain sensations (i.e., “the pain will not be cured or it will be worse”).
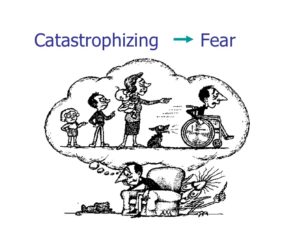
Pain catastrophizing is the tendency to describe pain experience in more exaggerated terms or to ruminate it. It has been defined as “an exaggerated negative mental set brought to bear during actual or anticipated painful experience” [2]. Pain catastrophizing and thinking about pain is strongly associated with intense experience of pain. Catastrophizing in relation to pain promotes fear of movement/ re-injury. Injury lead to experiences of pain and some tends to catastrophize, those who catastrophize develop pain related fear. Because of this fear they avoid the movement resulting disuse, depression and persistence of pain (chronic pain) leading to disability [3].
If the catastrophic thinking can be addressed, then the person's pain experience can also be reduced, which in turn might reduce health care utilization because it is a modifiable variable. Pain catastrophizing is one of the important psychological factors that predict post - operative pain [4]. PCS scores on the first post-operative day or in acute pain predict long term pain and disability in orthopedic surgery patients. This can guide the clinicians to adequately manage pain post operatively and also the patients can be timely informed about the prognosis.
Similarly assessment of catastrophizing can guide physiotherapists to better manage the pain and also to identify the group who can have chronic pain. Cognitive and behavioral interventions can be adopted at the early stage to reduce the disability and long term pain [5]. The primary treatment for pain catastrophizing is cognitive behavior therapy. Pain coping skills should be delivered to those who have more catastrophizing than other to reduce long term pain or disability.
So how can I assess pain catastrophizing in clinical practice?
To measure pain catastrophizing many of the measurement tools have been used such as: the Coping Strategies Questionnaire (CSQ), the Pain-Related Self-Statements Scale (PRSS) and the Cognitive Coping Strategy Inventory (CCS) and Pain Catastrophizing Scale (PCS). Among these, the PCS is widely used tool for the assessment of pain catastrophizing.
The Pain Catastrophizing Scale is a 13- item self-reported measure of pain catastrophizing assessing negative through associate with pain. The PCS measure three dimensions of catastrophizing: Rumination, Magnification, and Helplessness. Rumination subscale comprise the four items and measure the tendency to focus on pain related thoughts. The magnification sub-scale comprises three items that measure the tendency to exaggerate the unpleasantness associate with pain and expectation of negative outcomes. The six items of the helplessness sub-scale measure the tendency to adopt a helpless orientation in appraisal of pain. Participant reflect on past painful experiences and rate their feeling of pain on a 5- point Likert scale (0” not at all”, 4 “all the time’). PCS score ranges from 0 to 52, where high score indicate more pain catastrophizing [2].
The PCS has been translated into more than 20 languages. Recently it has been translated to Nepali language by Saurab and colleagues. The PCS can be completed and scored in less than 5 minutes, and thus it can be included as a part of routine clinical assessment especially for those with chronic pain. I am currently working with Saurab to validate this scale and assess its applicability among individuals following post- orthopedic surgeries. This tool is very useful in order to identify the psychological factors associated with pain and to identify those groups of patients who are likely to develop persistent disabling pain. If identified early, this can be prevented by cognitive behavioural and functional therapy.
References:
1. Davidhizar R, G.J., A review of the literature on care of clients in pain who are culturally diverse. International nursing review, 2004. 51(1): p. 47-55.
2. Sullivan M J L, B.S., Pivik J, The Pain Catastrophizing Scale: Development and validation. Psychol Assess, 1995. 7: p. 524-532.
3. Leeuw M, G.M., Linton SJ, Crombez G, Boersma K, Vlaeyen JW, The fear-avoidance model of musculoskeletal pain: Current state of scientific evidence. J Behav Med 2007. 30: p. 30:77-94.
4. Khan RS, A.K., Blakeway E Catastrophizing: a predictive factor for postoperative pain. Am. J. Surg, 2011. 201(1): p. 122–131
5. Williams, A.C., C. Eccleston, and S. Morley, Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev, 2012. 11: p. CD007407.
About Hari - He is currently an intern at the Department of Physiotherapy, Kathmandu University School of Medical Sciences. He has a keen interest in the assessment of psychosocial aspects of pain especially catastrophizing. He has the potential to be a leader in the physiotherapy profession in Nepal who has fine clinical skills, sound knowledge and excellent clinical reasoning.

