How can we measure pain?
The ultimate aim of any clinician is to relieve afflictions of the patient which is measured in terms of pain. Pain is a psychological phenomenon and naturally there are several facets central to its perception [6]. These include intensity, duration, interference with activities or disability, affect, tolerance, fear avoidance, catastropizing etc. There are multiple validated outcomes to measure each of these before mentioned aspects of pain [6]. Among these uni-dimensional self-reported measures of pain intensity are most frequently assessed in clinical practice as well as for research purpose [7]. There are various types of pain measures. These include:
1) Self-reported pain measures (scales, questionnaires),
2) Observational measures (function, ROM, activity limitation) and
3) Physiological measures (heart rate, respiratory rate, sweating) [11].
Since pain is a subjective experience, self-reported measures are considered "gold standard". Observational and physiological measures may be used in patients who are unable to effectively communicate (such as comatose patients and neonates) but they cannot be accurately used in chronic cases as the body adapts to the pain stimulus [11]. In this article, the self-reported measures of pain intensity will be discussed with their advantages and disadvantages.
Self-reported measures of pain intensity
The chief concern of any patient visiting a physician is pain [6]. So self-reported measures of pain intensity are recommended in minimum pain assessment [3; 6; 7]. The results are then used to classify patients for appropriate treatment based on pain response to movements or tests, measure the efficacy of treatment, and for prognostic purposes [3; 10]. There are a number of scales available to use for assessment of intensity. These include but are not limited to:
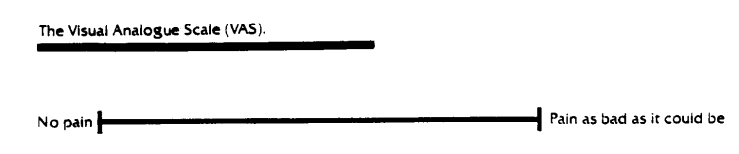
1. Visual Analogue Scale (VAS)
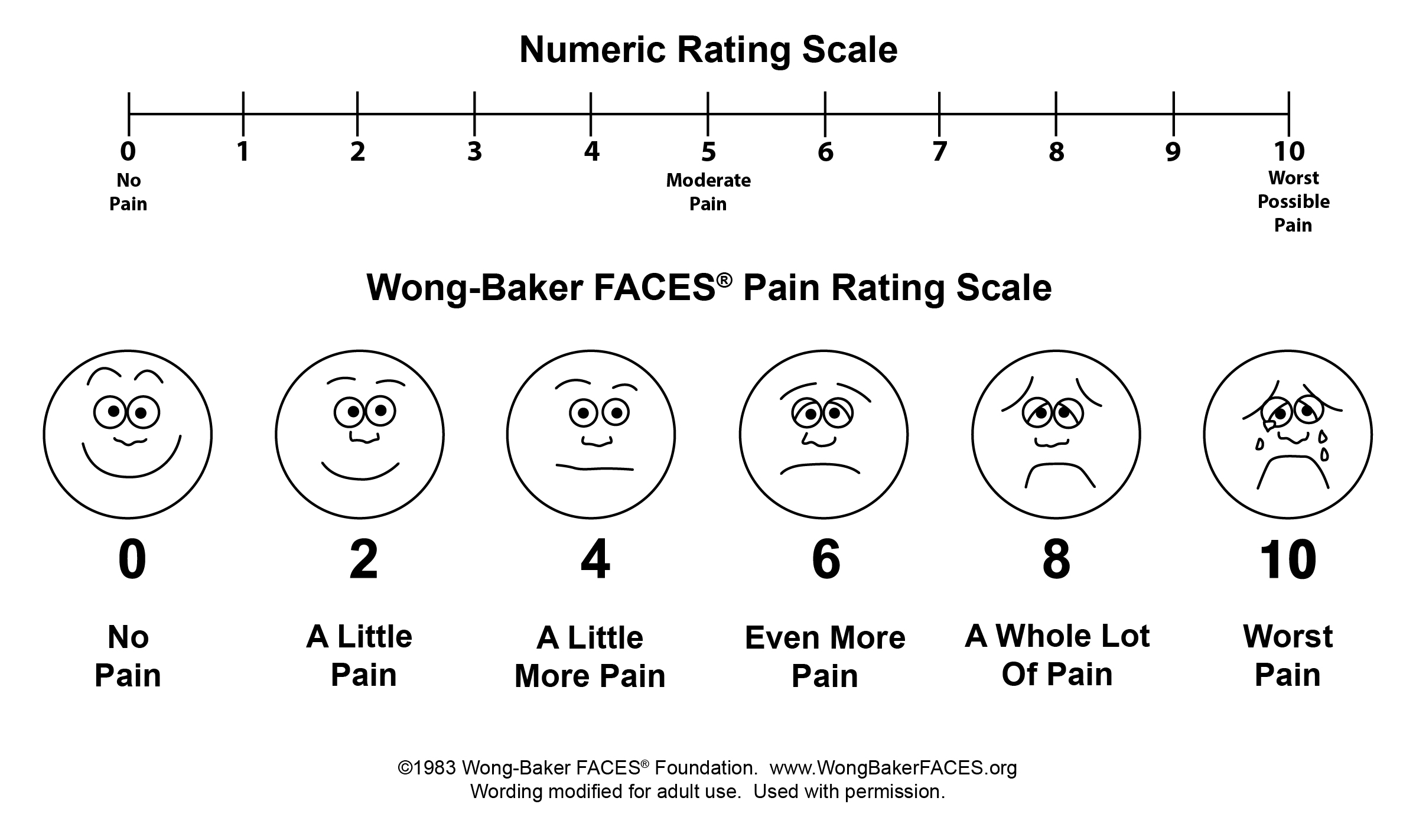
2. 11 point Numerical Rating Scale (NRS)
3. 4 point verbal rating scale (VRS-4)
4. 5 point verbal rating scale (VRS- 5)
5. Faces Pain Scale- Revised (FPS-R)
6. PROMIS- Pain Intensity scale
All of these tools possess good to excellent psychometric properties and are highly correlated with each other [6]. No gold standard has been established and researchers do not strictly demand the use of one over the others [7; 9]. However, several distinctions have been made regarding the merits and demerits of these scales. These are summarized below:
VAS:
- It is a ratio scale which is very important as it can be analysed as continuous variable and parametric tests can be used to analyse.
- Electronic VAS and mechanical VAS are available and are shown to correlate highly with paper VAS [6; 7].
- Most frequently used tool in research studies so allows for comparison between studies [7].
- Allows for end number of responses which is why it is considered more sensitive compared to other scales [13].
Disadvantages:
- Scoring is more time consuming
- Liable to measurement errors
- Cannot be done over telephone
- Is more difficult to understand [6] and
- Is less applicable in elderly and in those with cognitive impairments [7].
NRS:
Advantages:
- Can be administered verbally and also can be administered by a telephone call. Thus it can be used in research of this nature [6]. It is also preferred by patients in different cultures [7].
Disadvantages:
- Patients who are inexperienced have a tendency to answer in multiples of '5' [6].
- Limited number of responses
VRS:
Advantages:
- It is easy to understand and can be administered verbally [6]. It is preferred by less educated and elderly [7].
Disadvantages:
- Has limited number of responses, so subject may have difficulty selecting one that exactly describes his/her pain.
- Terms are interpreted differently by individuals.
- Is an ordinal scale, so conclusion about magnitude of change in pain is hard to interpret [6].
Faces Pain Rating Scale:
Advantages:
- Preferred scale in those with cognitive impairment [14] and for assessment of pain in children.
Disadvantage:
- Has only been validated for few adult conditions.
PROMIS Pain Intensity
Advantages:
- Have demonstrated high measurement precision and is also available as a short form [1,2].
Disadvantages:
- Requires 7 day recall and the scoring is complicated [1].
Considerations for pain intensity assessment
• Pain intensity is liable to change. Recent studies recommend the use of composite scores (at least 2 ratings is reliable and valid) and asking the person to rate their ‘usual pain’ on an average of 24 hours to 1 week and the ‘current pain’ [6; 8].
• For a comprehensive evaluation of pain -- pain interference, pain affect, pain tolerance, pain acceptance, catastropizing, etc should also be assessed [6].
• Most research on pain intensity measures are done in the western population and use NRS as a standard outcome [4; 5; 7]. However, majority of the Nepalese population are illiterate, so a numerical scale is probably less suited for our patients.
• There may be differences among physicians and patients about which intensity the pain is bearable. So it is good to ask the patient if he considers the pain bearable along with use of a pain intensity measure tool [4].
• It should be born in mind that these measures rely on a person’s ability to communicate [11]. Hence, proper explanations should be given regarding the use of the scales.
Summary
All of the above mentioned scales have their own merits and demerits so preference for a scale is based on the clinicians’ own clinical decision making and patient’s preferences. Composite scores are better than asking for just “current” pain. Clinicians should talk to the patient regarding what intensity they find bearable and when change in intensity is significant for them. Also, pain intensity should not be used as a sole measure of pain assessment and other facets of pain should also be assessed as mentioned above. Pain intensity assessment can be quite deceiving in especially chronic pain which is ruled by central sensitization.
References:
[1] PROMIS pain intensity scoring manual. https://wwwassessmentcenternet/documents/PROMIS%20Pain%20Intensity%20Scoring%20Manualpdf.
[2] Broderick JE, Schneider S, Junghaenel DU, Schwartz JE, Stone AA. Validity and reliability of patient-reported outcomes measurement information system instruments in osteoarthritis. Arthritis Care Res (Hoboken) 2013;65(10):1625-1633.
[3] Deyo RA, Dworkin SF, Amtmann D, Andersson G, Borenstein D, Carragee E, Carrino J, Chou R, Cook K, DeLitto A, Goertz C, Khalsa P, Loeser J, Mackey S, Panagis J, Rainville J, Tosteson T, Turk D, Von Korff M, Weiner DK. Report of the NIH Task Force on research standards for chronic low back pain. J Pain 2014;15(6):569-585.
[4] Dijk JFMV, Wijck AJMV, Kappen TH, Peelen LM, Kalkman CJ, Schuurmans MJ. Postoperative pain assessment based on numeric ratings is not the same for patients and professionals: A cross-sectional study. International Journal of Nursing Studies 2012;49:65-71.
[5] Farrar JT, Young JP, Jr., LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94(2):149-158.
[6] Haefeli M, Elfering A. Pain assessment. Eur Spine J 2006;15 Suppl 1:S17-24.
[7] Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, Fainsinger R, Aass N, Kaasa S. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage 2011;41(6):1073-1093.
[8] Jensen MP, Hu X, Potts SL, Gould EM. Single vs composite measures of pain intensity: relative sensitivity for detecting treatment effects. Pain 2013;154(4):534-538.
[9] Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain 1986;27(1):117-126.
[10] O'Sullivan P, Waller R, Wright A, Gardner J, Johnston R, Payne C, Shannon A, Ware B, Smith A. Sensory characteristics of chronic non-specific low back pain: A
subgroup investigation. Man Ther 2014;19(2014):311-318.
[11] Strong J, Sturgess J, Unruh AM, Vicenzino B. Pain assessment and measurement. Pain : a textbook for therapists 2002;Section 2.
[12] Sullivan MD, Ballantyne J. Must we reduce pain intensity to reduce chronic pain. Pain 2015;epub ahead of print.
[13] Valente MAF, Ribeiro JLP, Jensen MP. Validity of four pain intensity rating scales. Pain 2011;152(2011):2399-2404.
[14] Ware LJ, Epps CD, Herr K, Packard A. Evaluation of the Revised Faces Pain Scale, Verbal Descriptor Scale, Numeric Rating Scale, and Iowa Pain Thermometer in older minority adults. Pain Manag Nurs 2006;7(3):117-125.