Reflection on the “Mulligan Concept” Workshop

It is very important for all clinicians to reflect on things that we learn may it be by undertaking a course or what our patients teach us every day in the clinic. By reflection, I mean, analyzing what did I learn, what is good about this, how can I use this in my patients, how will it change the outcome of my future patients and also why can I not use this technique for my other patients. It would also be good to ask other participants in a course like this about what is the best thing that they learnt and can be used. I think this is the best way to develop our reasoning process. Here, I will reflect on the “Mulligan Concept” workshop I recently attended.
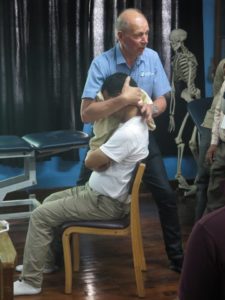
A three-day Mulligan Concept workshop was organized by Dhulikhel Hospital between 18th to 21st March, 2016. Jack Miller (from Canada) and Timothy (Tim) Mann (from Australia) members of Mulligan Teachers’ Association and accredited Mulligan teachers volunteered to come to Nepal for this. The workshop was assisted by Phil Shepherd. Mulligan concept is an important manual therapy tool that can help our patients achieve pain-free function/ full range of function and improve the overall function utilizing numerous techniques.
The first day on 18th, Tim taught our brilliant third and fourth year students who were successful in learning the handling skills in Mulligan concept quickly. Jack and Tim spent the next three days with physios from all over Nepal with a participant from African continent. Jack mostly spent the first day talking about the foundational pillars of Mulligan concept which also are the components of Evidence Based Practice (EBP) which are (1) clinical research; (2) clinical reasoning; and (3) patients’ values (their expectations and preference). Jack also highlighted that how the concept evolved and how it can be effective to variety of clinical conditions or painful sites with available science behind the effectiveness of the Mulligan’s manual therapy.
Personally for me, it was very important that the experts emphasized on the importance of clinical reasoning and identifying the patients who benefit from this form of management from clinical research (clinical prediction rules) and also value other treatment approaches. For example on the first phase of management, pain control is important, then the focus would shift towards making patients more active and teaching self-management and home exercises, finally moving towards other advanced goals such as improving the strength, flexibility, aerobic capacities etc. Thus, it is important to understand what stage of healing (acute versus chronic) the patient is at and using sound clinical reasoning to plan the right treatment with patient in the center of the planning. I will divide this blog post into two parts based on what I thought was the most important message the expert left with us (though there are many others too) so that I can share this with my friends and colleagues who did not get an opportunity to attend the course.
(1) Physios do not treat a pathology but treat impairments and work to improve function based on assessment findings
(2) Physio do not treat pain just to treat pain but to improve function
(1) Most of us who are trained on the “patho-anatomical model” find it very difficult to determine the physiotherapy treatment approaches for patients. I keep getting asked from my physio friends “hey tell me how exactly I can treat an OA knee?”, “what is the best treatment for cervical spondylosis?”, I also had my friends send me MRI scans of low back with suggestions for correct forms of exercises and my physio colleagues also post “X-rays” of spine on social media to seek for advices on the “treatment of the patient”.
I can understand how difficult it was for Jack and Tim to explain that “we don’t treat a pathology”. They explained this to the group, talked to each participant individually, and to the same person many times. Jack described this as being self-trapped in the “patho-anatomical model” for physiotherapy management is like keeping ourselves trapped inside a “pathology jail” and we have a key to get out of it, and we can only get out of it only if we want. This metaphor is an excellent way to explain how important it for us to stop asking others ways to treat cervical myelopathy, stroke or ankle sprain; but start assessing the patient, identify impairments, functional limitations, psycho-social impacts of the problem and start addressing them with primary therapeutic goals. Jack explained that he was out of this “pathology jail” long back, I came out of this (and please believe me that I felt enlightened to be out of this “jail”) in 2010. When ideas get embedded in head for a long time, it takes longer time to delete it. But it is easy only if we are open to new ideas, think about it logically, search for the evidences behind it and them update ourselves.
What this means is, understanding that we do not treat an OA knee – but instead we should assess a person with knee pain, to (1) identify the impairments (loss of terminal knee extension/ flexion, inadequate patellar mobility, inability of the quadriceps to relax due to hell a lot of static quadriceps exercise versus weak quadriceps, weak hip and calf muscles etc); (2) identify functional limitations that the patient is having; (3) identify central contribution of the pain such as cognition and thought processes, fear of movement, catastrophizing, anxiety, depression, sleep that is modulating the pain; (4) identifying if patient is affected by any social factors that is maintaining the pain (e.g., family members keep telling the a woman with lateral elbow pain that it will get worse, the arm will turn gangrenous and need amputation just like her father in law’s friend – this is a real example) and how much this pain interferes with the social participation. The management for someone with above problems would be manual therapy to improve the range of motion that is affected and exercises to maintain the improved range, strengthening of the calf and hip muscles which are weak, addressing the psychosocial factors including fear of movement by assurance, education and coping strategies and working on to make the individual functional. Trust me in this that every patient with OA knee will have different reasons for pain even if they are of same age, sex, same stage of OA, and even if they have x-rays that look exactly the same. It is also important to understand that imaging such as x-rays and MRI do not correlate with the amount of pain the person has. Those who have very bad x-ray may have no pain at all, and those with no problems or minimal problem in x-ray can have severe intensities of pain. Thus, rather than relying on x-rays or pathology model, physios will require to assess every patient individually and plan appropriate goal of management for that patient based on their own individual assessment findings and clinical reasoning utilizing the best available evidences and respecting patient’s values. Like Jack said, scans are important for us but not to tell us what treatment to give to the patient but to inform us “what not to do on the patients” which could be red flags or contraindications to our manual assessment and treatment.

(2) When a person has a pain because a thorn is stuck on the sole of the foot – how will you manage this patient? Would you use TENS to reduce pain, or ultrasound and hot pack to improve circulation? Ice because it is acute and it will heal the problem faster? Or pain killers because the pain is so much that it interferes with the person’s activities?
Using one or all of these can be options for pain management should be fine but the patient will not improve, but the first thing that is logical would be to remove the “thorn” from the person’s foot. Every patient will have a similar “thorn” that is maintaining their pain which could be “fear of movement”, “wrong beliefs about the diseases” thinking that the disease is severe and will never get treated and will get worse”, “excessive loading to the bodily tissues while work”, “wrong ways of exercise”, “no exercise”, “hell a lot of sitting” etc. These causes of pain should be removed first, and then we manage the pain by our favourite “pain management modality”, strengthen weak muscles, move stiff joints, stretch tight muscles. That is why thorough assessment of bodily structures “bio”, psychological state “psycho” and social contribution “social” (together bio-psycho-social) is so important.
At the end of the course, I think at least half of us have come out of the “pathology jail” like Jack did more than a couple of decades back, I did six years back; and we who are out of this jail should help others free themselves. Also, practicing what we learned as skills after the course is important to master it so that we move from “conscious competency” stage to “unconscious competency” with practice, practice and more practice.
I thank Jack and Tim for coming to us to spread this important message which is I think the first and most important thing to learn before we learn any advanced skills. I will be happy to help anyone with the best of my abilities. I am sure, Jack and Tim will be happy to help us too. Thumbs up to the organizing team for their commitments to bring the experts to Nepal and for organizing an excellent workshop.
To conclude, 48 physios and 43 physio students are now trained in Mulligan concept in Nepal in a very low cost of participation by the leading expert in the field; and I am sure a lot of patients will benefit; and those who underwent the training will teach their colleagues so that more and more of us starting using the concept.
