Assessment of Pain in clinical and experimental setting
Pain assessment has always been a challenge for researchers for many years. They have always tried to quantify pain. Quantitative sensory testing (QST) evaluates the integrity of the entire sensory receptors. It is found to be a reliable and relatively reproducible. Though QST is a subjective test, recent brain imaging studies provide strong evidence that subjective pain scores are associated with objectively measured neural activity in the brain that are known to be involved in pain processing. This gives us a clue that QST can indicate the changes in the brain due to pain.
QST is used clinically to diagnose disorders related to peripheral small fibers and disorders of sensation (both peripheral and central). This assessment is of value when an anatomical lesion is not detected by imaging. This article will focus on the assessment of pain using QST in people with pain and in healthy volunteers.
The various modalities used for assessing sensations are: heat, cold, mechanical, electrical and chemical. The pain assessment using QST can be performed to diagnose pain as a result of disease and to identify the mechanisms of pain among healthy subjects.
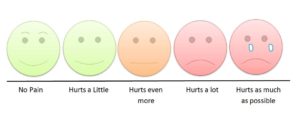
1) Assessment of painful conditions: Spontaneous pain in various painful conditions can be assessed using various scales such as Visual Analogue Scale (VAS), Numerical Pain Rating Scale (NPRS) and Verbal Rating Scale (VRS). Both NPRS and VAS are commonly used tools in research and clinical practice. VRS is valuable for those who find difficulty to explain their pain sensations in numbers. These measures give us valid and reliable assessment of pain intensity.
Assessment of quality of pain: Assessment tools such as McGill Pain Questionnaire can be used to assess the quality of pain. From the literature it is clear that different painful conditions have different words to explain their quality of pain. For example people with neuropathic pain explain pain more as burning. We do not yet know in Nepal, what words to different people use to explain their painful conditions.
Assessment of neuropathic pain: Various tools can be used to assess neuropathic pain such as Leads Assessment of Neuropathic Symptoms and Signs (LANSS). Self- reported version of LANSS can also be used. There are many other tools that can be used to assess neuropathic pain which will be addressed in a separate article.
Assessment of experimental pain: Pain can be provoked experimentally in various ways such as using pressure, electricity, heat and cold. During these painful experimental processes, different parameters can be assessed including pain threshold and pain tolerance.
Pain Threshold: One way of testing threshold is by using “method of limits” in which the stimulus is given to the point at which subject experiences the onset of pain. Here, the time required to elicit response may vary among individuals based on various characteristics such as age, sex, ethnicity etc. Another method called “staircase family of test” is used where stimulus of pre-defined intensity is provided and the person is asked if it is painful or not.
Tolerance: It is the stimulus up to which the subject can tolerate pain. It can be measured by using cold stimulus by asking the subject to immerse limb in cold water and hold it as long as they can.
Supra threshold stimulus: It is the stimulus beyond threshold required to elicit a response. The stimulus can be given as double the intensity of threshold or the same intensity of threshold but with increased duration. Subject’s response can be measured by VAS, NPRS or VRS.
Summation: The perception of pain depends on the summation of incoming information to the brain. It can be measured as two of the following:
Temporal summation: It is the process in which the repetitive stimulation of small diameter primary afferent fibers produces increase in action potential discharge by the activation of NMDA receptor-dependent channels. Prolonged stimulation of such fibers causes sensitization of these neurons known as temporal summation. Further sensitization of the neurons leads to allodynia and hyperalgesia with decrease in pain threshold. Temporal summation can be examined by using various modalities (mechanical, thermal, electrical) to elicit pain. The principle is that the repetitive painful stimulus which is given at fixed intensity or a painful thermal stimuli given for long duration. In both methods, the difference of first and last stimulus is taken as a measure of temporal summation.
Spatial summation: It is “the ability to integrate painful stimulus from large areas of the body”. It refers to the number of central neurons activated and thus the size of the stimulated area.
Clinical application of summation:
Since enhanced “wind-up” contributes to neural processes that lead to hyperalgesia and persistent pain, temporal summation can be used to assess altered pain processing in chronic pain patients.
Clinical uses of QST:
- QST can be used to diagnose various abnormalities of sensory afferent fibers, differentiate between neuropathic and non-neuropathic pain, CRPS type 1 and 2, diabetic neuropathy and orofacial pain.
- For assessment of patterns of pain responsiveness and prediction of clinical pain.
- It can also be used to assess the severity of pain syndromes.
- It can be used for understanding of various pain mechanisms such as central sensitization.
- It can be used to assess the efficacy of an intervention by testing before and after the intervention.
- It can also be used to track if the neuropathic features of pain are alleviated.
Summary:
Pain is one of the major and inseparable sensations which hinder one’s lifestyle and normal functioning. So, to address or to treat pain, careful assessment of pain is necessary in order to understand the underlying mechanisms of pain. Identifying central pain versus nociceptive pain versus neuropathic pain is important before we can use any interventions for pain management. QST has been established as a valid and reliable tool to assess pain (with variety of other sensations), it’s type, severity and follow up changes and response to treatment.
Reference:
David Yarnitsky and Michal Granot. Neurophysiological assessment of Neuropathic Pain; Chapter 27 – Quantitative Sensory Testing. Handbook of clinical neurology. 2006.
About Jyoti: She is a fourth year Bachelor of Physiotherapy Student at Kathmandu University School of Medical Sciences. She is passionate about neurology and how brain can contribute to pain. She is interested to explore the contribution of central sensitization in musculoskeletal pain.

